Egg quality is a crucial factor in reproduction. It refers to the genetic integrity (DNA), maturation, and overall health of an egg. As women age, DNA integrity declines, reducing the chances of having a healthy baby. This article explores the factors influencing egg quality, its assessment, and its impact on IVF outcomes
Factors Affecting Egg Quality
Several factors influence egg quality, with maternal age being the most significant.
- Maternal Age
As a woman ages, the eggs she is born with undergo genetic degradation, increasing the likelihood of chromosomal abnormalities in embryos. These errors occur mainly at ovulation and are not affected by hormonal medications, diet, or stress. During ovulation, eggs reduce their chromosome count by half (from 46 to 23 chromosomes) to make room for the 23 chromosomes contributed by sperm during fertilization. The percentage of genetically normal embryos declines significantly after age 35, emphasizing the importance of age in IVF success rates and egg freezing.![]()
![]()
Graph 1: Proportion of Euploid Embryos per IVF Cycle by Maternal Age (Demko Fert & Steril 2016)
- Polar Body and Cumulus Cells at Egg Retrieval
During ovulation, half of the egg’s original DNA is expelled into a small polar body, while the remaining half is retained. The integrity of this polar body and the protective cumulus cells surrounding the egg are indicators of egg quality. Intact polar bodies are associated with higher fertilization rates in IVF. Cumulus cells, which support egg maturation, can be observed after egg retrieval and also provide insight into an egg’s developmental potential.Ovulation divides the original egg DNA by half. During that genetic division, one side retains the original “hardware” while the extra 23 chromosomes are expelled into a small polar body. The integrity of this polar body and protective cumulus cells surrounding the egg are additional indicators of egg quality and integrity. Intact polar bodies are often associated with higher fertilization rates during IVF. Cumulus cells, which provide essential support to the egg during maturation can easily be seen after egg retrieval and also serve as an indicator of the egg’s potential to develop into a healthy embryo. - Lifestyle and Environmental Factors
Although women are born with a fixed number of eggs, external factors such as smoking, chemotherapy, and radiation can impact egg quality. Smoking, for instance, can reduce IVF pregnancy rates by up to 50%. It is recommended to quit smoking or switch to nicotine products (without tar) to support detoxification and potentially improve outcomes.
Assessing Egg Quality
There is no direct blood test to assess egg quality (DNA). Egg quality can only be determined once eggs are retrieved during IVF, which is one reason why many patients are classified as having “unexplained” infertility. Eggs are not typically graded themselves; rather, when fertilized eggs become embryos and reach the blastocyst stage (generally on Day 5 or 6, with about 120 cells), they can be evaluated based on appearance or genetically tested with PGT. At age 36, only half of surviving embryos are genetically normal, underscoring the challenge brought by impaired egg quality.
- Hormone Levels
Hormones such as Anti-Müllerian Hormone (AMH), Follicle Stimulating Hormone (FSH), and estradiol help assess egg quantity, but not the genetic health of the egg. - Menstrual Cycles
Regular menstrual cycles do not indicate better egg quality (or quantity). Women with irregular cycles (PCOS) may have lower egg quality compared to normally ovulating women but egg quality can impact women with regular cycles too. Glucophage (Metformin) can help fix insulin resistance and reduce miscarriage rates, but its benefits primarily affect the uterine environment not the DNA integrity of eggs. - Previous IVF Success
Success in previous IVF cycles, particularly with good embryo development, is a strong indicator of good egg quality. Women who have achieved successful fertilization and embryo development in past IVF attempts are more likely to have healthy eggs in subsequent cycles if they remain in the same age group.
Egg Quality and IVF Outcomes
In IVF, egg quality significantly influences the chances of a successful pregnancy. Mature eggs, particularly those at the metaphase-2 (M2) stage, are ideal for fertilization and yield the best outcomes. The 2022 SART data is pictured below. Please note that comparing clinic success rates is misleading because patient characteristics and treatment methods vary by clinic. For example, clinics that discriminate against poor candidates would have a lower pregnancy rate.
In women above the age of 35, genetic testing can improve pregnancy rates by identifying those embryos that are most likely to make a baby. The additional cost may negate the advantages for some couples. IT IS IMPORTANT TO UNDERSTAND THAT THE TESTED CELLS MAY NOT BE REPRESENTATIVE OF THE WHOLE EMBRYO. There is a 10% false positive and 10% false negative rate. For example, at age 40, the risk of Down’s syndrome is around 1%. Because the test is only 90% accurate, the risk of Down’s would be 1/1000. Testing every cell in an embryo would damage it and limit the usefulness of such a test. Also, as the graph indicate, even when tested the live birth rate is still around 50%.
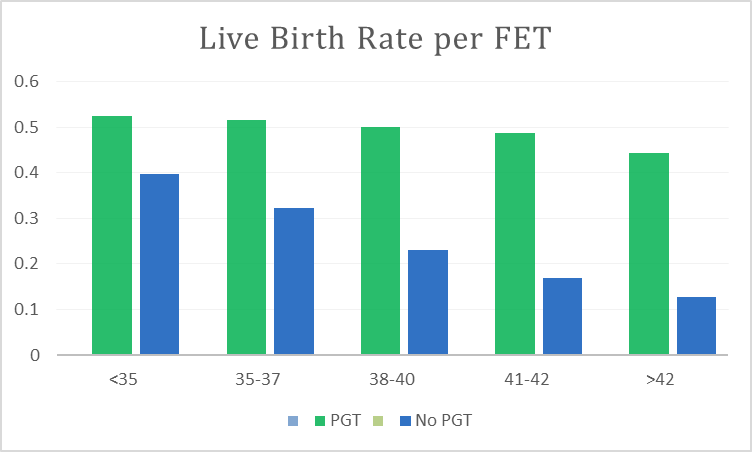
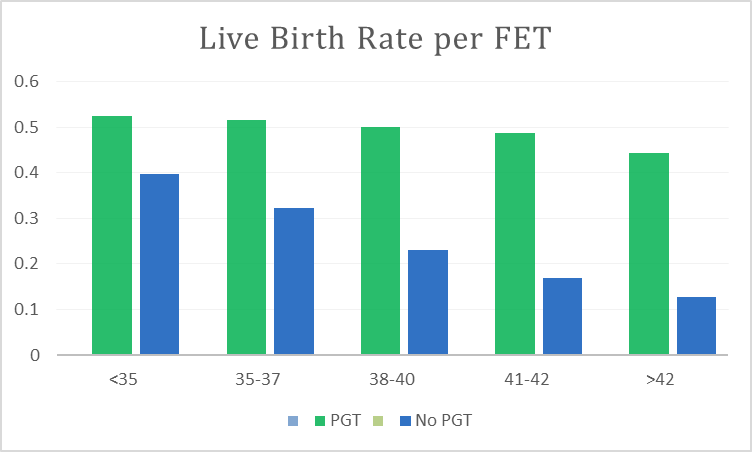
Graph 2: Live Birth Rates per ET. SART.org Data 2022
Conclusion
Understanding the factors affecting egg quality helps women make informed fertility decisions regarding the option with the best chance of a healthy baby. Age-related chromosomal errors are the most significant determinant of IVF success. Women under 35 have a higher percentage of normal eggs and euploid embryos, increasing their likelihood of successful IVF outcomes. In this age group, preimplantation genetic testing (PGT) is generally unnecessary. In contrast, women over 35 have a higher proportion of abnormal eggs, leading to lower success rates, increased miscarriage risks, and higher chances of chromosomal disorders. To avoid future fertility challenges, egg freezing before age 35 is advised.
Many women over 42-43 consider using donor eggs, particularly when their ovarian reserve is low. IVF is generally not recommended for women over 44 due to its low success rates. It is important to understand that egg quality and fertility cannot be significantly enhanced by supplements, hormonal treatments, or stress relief methods because they do not restore DNA inside the egg.