Starting or growing a family after 40 is increasingly common, driven by factors like career, finances, or finding a partner later in life. Fortunately, advancements in fertility treatments, especially in vitro fertilization (IVF), offer a safer path to parenthood in that age group.
It’s crucial to understand the biological factors and potential challenges involved before making the right choice. This post will delve into key considerations such as AMH levels (egg reserve), chromosomal risks, miscarriage rates, and how PGT (pre-implantation genetic testing of embryos) can help improve the likelihood of a healthy pregnancy.
Fertility After 40: What Changes?
Female fertility declines steadily with age due to both the quantity and quality of eggs. Women are born with 1–2 million eggs, and this number decreases sharply over time. By puberty, around 400,000 remain. After 35, the decline accelerates, and by 40, the remaining eggs are fewer — and less likely to be genetically normal.
AMH Levels Over Time
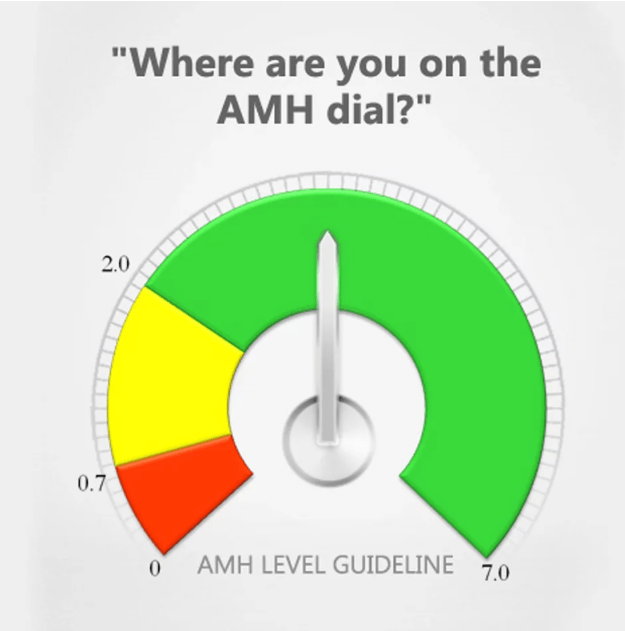
Anti-Müllerian Hormone (AMH) is one of the most reliable lab markers for ovarian reserve — or how many eggs a woman has left. AMH doesn’t measure egg quality, it only measures quantity, just like a “gas tank”.
AMH naturally declines with age and may become undetectable in perimenopause. Women over 40 often have low AMH, which can mean fewer eggs retrieved during IVF, but pregnancy is still possible — especially with careful monitoring and personalized treatment plans.
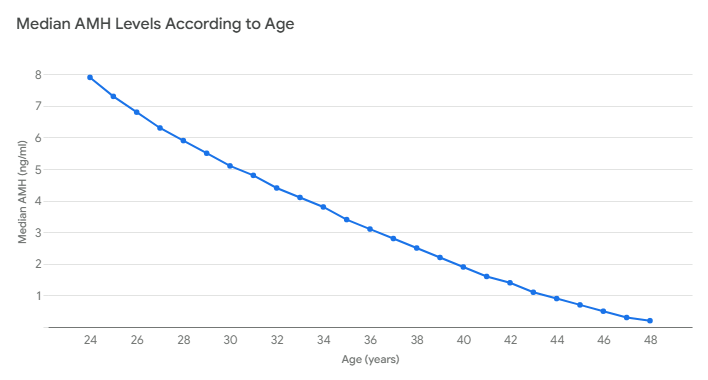
Reference: Seifer DB, Baker VL, Leader B. Age-specific serum anti-Mullerian hormone values for 17,120 women presenting to fertility centers within the United States. Fertil Steril. 2011; 95 (2): 747-50.
Egg Quality and Euploidy: The Real Challenge
While egg quantity declines, egg quality — specifically, the number of genetically normal eggs — is often the biggest hurdle.
What Is a Euploid Egg?
During ovulation, an egg splits its number of chromosomes from 46 to 23. A euploid egg has the correct number of chromosomes (23). As women age, the chance of making an error during ovulation increases. As a result, the risk of producing an aneuploid (abnormal) egg increases, which contributes to infertility, miscarriage, and birth defects such as Down syndrome. The DNA error rate is not related to diet, exercise or stress. It is part of the normal aging process.
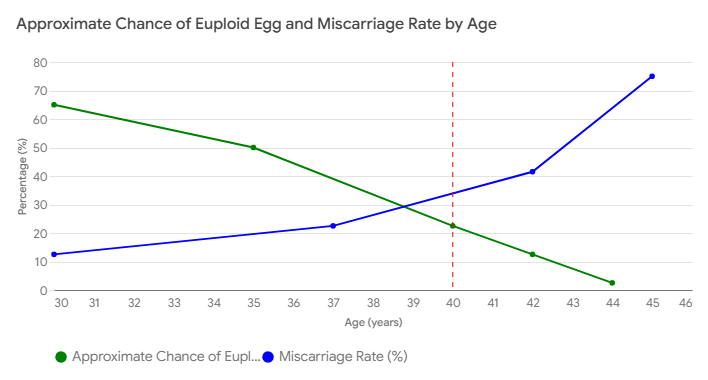
As a result, a woman over 40 may may need multiple eggs or IVF cycles just to create one healthy embryo for transfer.
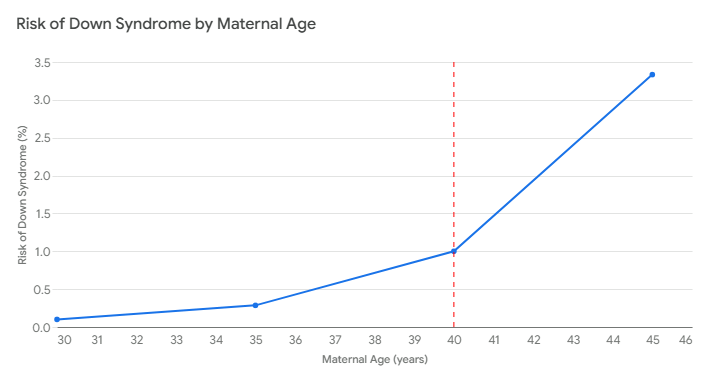
Chromosomal Risks & Down Syndrome
Chromosomal abnormalities rise steeply with age, increasing the risk of genetic conditions like Trisomy 21 (Down syndrome). These risks are directly tied to the quality of the egg. Sperm quality declines more slowly with age, but egg chromosomes are more fragile and prone to errors in older women.
Miscarriage Rates Over 40
When conception occurs with an abnormal embryos, the embryo stops growing, causing a miscarriage. Most miscarriages occur in the first trimester and are due to chromosomal errors. IVF with PGT-A allows genetic screening before implantation, helping reduce that risk of miscarriage in older women.
Pregnancy Complications in Advanced Maternal Age
Women over 40 face higher risks of pregnancy complications, even with a healthy embryo. These include:
- Gestational diabetes
- High blood pressure/preeclampsia
- Placenta previa or abruption
- Low birth weight
- Preterm labor
- Increased C-section rates
Because of these inherent risks, most unrelated to IVF itself, more pregnancies after 40 are classified as high-risk and are followed closely, sometimes with the help of a maternal-fetal specialist.
IVF Over 40: How It Helps.
IVF with PGT is often the safest pathway to conception for women over 40.
1. Embryo Banking & Multiple Retrievals
Since fewer eggs and embryos are expected in each IVF cycle over 40, many patients undergo multiple cycles to bank normal tested embryos, improving the odds of success later in life when a second child is desired and when euploid embryos are more difficult to obtain.
2. PGT Genetic Screening
Preimplantation Genetic Testing for Aneuploidy allows for screening embryos before implantation. Only euploid embryos are transferred after IVF with PGT, reducing miscarriage rates and improving live birth rates.
3. Donor Eggs
If a woman’s own eggs can’t produce a healthy embryo, donor eggs from younger women provide dramatically higher success rates — often exceeding 50–60% per IVF cycle, regardless of the recipient’s age.
IVF Success Rates Over 40 (With and without PGT)
According to the CDC’s National ART data, pregnancy and live birth rates for women using their own eggs and not using PGT are as follows.
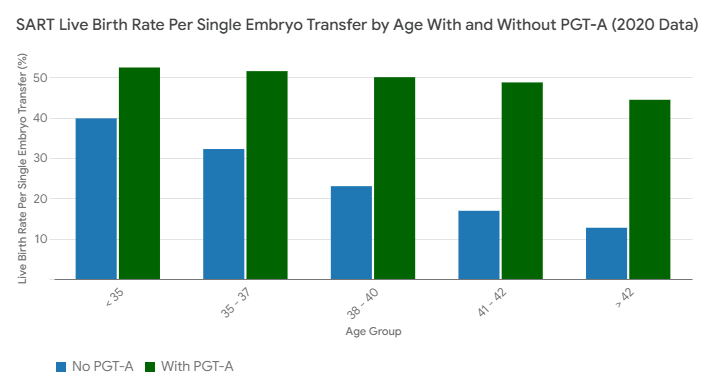
The data presented in this graph is from the 2020 SART public outcome tables.
These figures emphasize the steep decline in success with age. IVF with PGTi mproves per-embryo transfer success rates because it selects the embryo that has the best chance of making a live baby. The chance of finding a euploid embryo is still the same and still limited by age and egg quality
Emotional and Financial Considerations
IVF can be physically, emotionally, and financially draining — particularly over 40, when more cycles may be needed to obtain a euploid embryo. Many women over 40 benefit from counseling, support groups, and honest discussions with their fertility doctors about prognosis and options like donor eggs, embryo adoption, or gestational carriers when needed.
Conclusion: Know Your Options, Plan Ahead
Getting pregnant safely after 40 is possible — but it often requires time, resources, and medical support. Understanding your AMH levels, egg quality, and the chances of finding a euploid embryo is essential for making informed decisions.
IVF with genetic screening gives older women the best shot at a healthy pregnancy, but expectations must be discussed. If you’re over 40 and hoping to conceive, consult a reproductive endocrinologist early. With the right approach and support, your path to parenthood is still very much within reach.