If you’re struggling to conceive or carry a pregnancy to term, and your doctor has mentioned a “uterine anomaly” or “Müllerian anomaly,” you’re not alone—and you’re certainly not without hope. Müllerian anomalies are congenital conditions that affect the development of a woman’s reproductive tract. They can have a direct impact on fertility and pregnancy outcomes. Thankfully, with modern diagnostics and treatment options guided by organizations like the American Society for Reproductive Medicine (ASRM) and the European Society of Human Reproduction and Embryology (ESHRE), many women with these anomalies can go on to have healthy pregnancies.
What Are Müllerian Anomalies?
Müllerian anomalies are congenital malformations that occur when the Müllerian ducts (the embryologic structures that form the uterus, fallopian tubes, cervix, and the upper portion of the vagina) don’t develop or fuse properly. These conditions are estimated to occur in up to 4–7% of the general female population, but they are more commonly found in women with infertility or recurrent pregnancy loss (up to 18%).
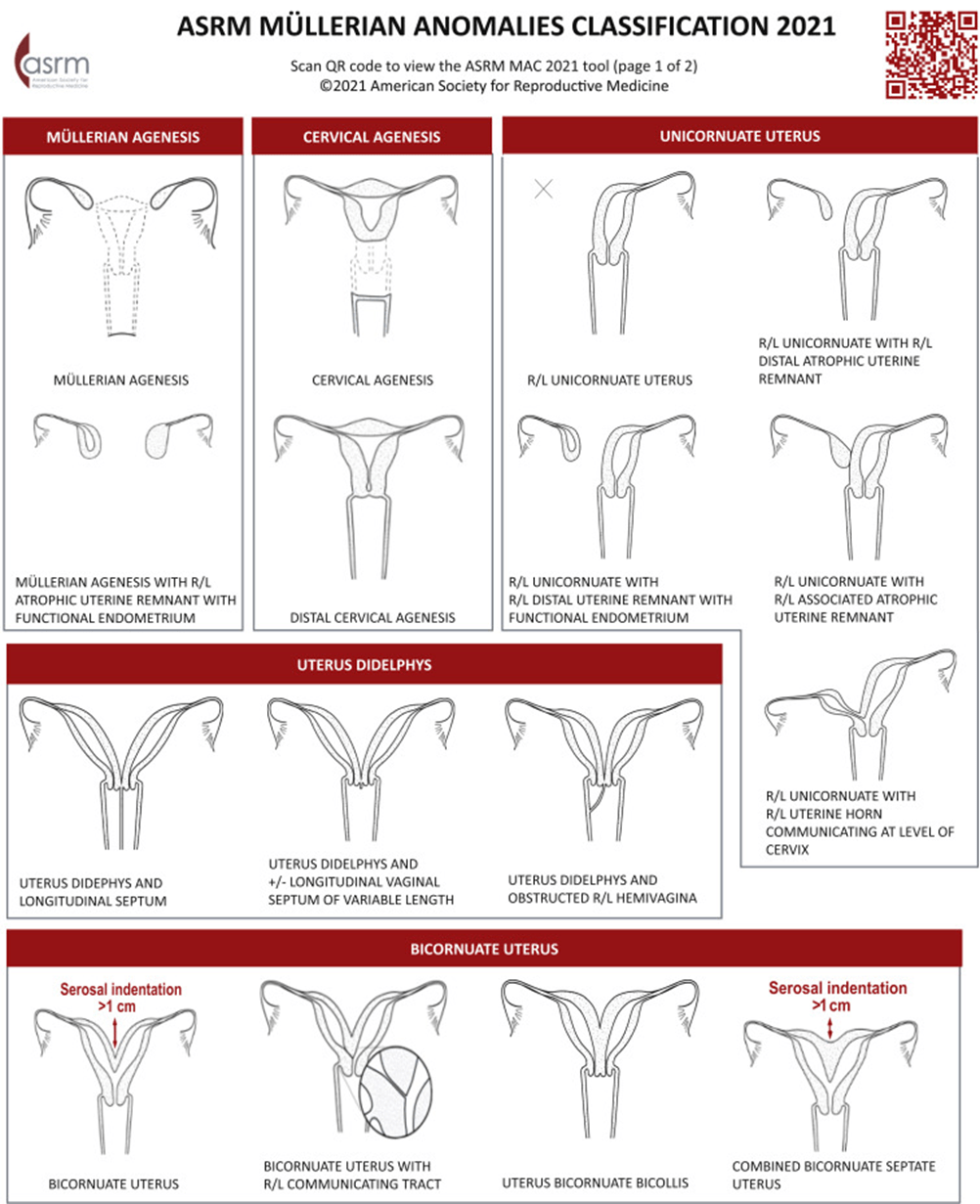
There are several types of anomalies, and they are usually classified by the ASRM and ESHRE into categories such as:
- Septate uterus – a fibrous or muscular wall divides the uterus, often leading to miscarriage.
- Bicornuate uterus – a uterus with two separate compartments or “horns”
- Unicornuate uterus – one-sided uterine development, often with a rudimentary horn.
- Uterus didelphys – two separate uteri, each with its own cervix (and sometimes a double vagina).
- Arcuate uterus – a mild indentation at the top of the uterine cavity; usually doesn’t require treatment.
- Aplastic or hypoplastic uterus (Mayer-Rokitansky-Küster-Hauser Syndrome) – absence or underdevelopment of the uterus.
How Do These Anomalies Affect Fertility and Pregnancy?
The impact varies widely depending on the type of anomaly:
- Arcuate Uterus, a normal variant with no effect on reproductive outcome
- A septate uterus, the most common abnormality, is strongly associated with recurrent miscarriage and infertility.
- A bicornuate or unicornuate uterus may result in preterm labor, malpresentation (e.g. a breech baby), or second-trimester loss.
- A uterus didelphys may support normal pregnancy, but some women experience miscarriage or preterm birth.
- Aplastic uterus typically results in absolute infertility, though options like gestational surrogacy or uterine transplant may be considered in the quest to have a child.
Diagnosis and Evaluation
Diagnosis typically includes a combination of imaging and diagnostic procedures:
- 3D transvaginal ultrasound – first-line tool for structural assessment, but few facilities in the DFW metroplex have the capacity to offer this
- Sonohysterography (saline infusion ultrasound) – helps delineate the shape of the uterine cavity.
- MRI – considered the gold standard for complex anomalies.
- Hysteroscopy or laparoscopy – sometimes used to confirm diagnosis or perform treatment.
Both ASRM and ESHRE recommend accurate classification and individualized assessment before treatment.
Treatment Recommendations (ASRM and ESHRE Guidelines)
Treatment is only advised when a Müllerian anomaly is clinically significant, especially when linked to infertility or pregnancy loss. Here are the key evidence-based approaches:
1. Septate Uterus
- Hysteroscopic metroplasty (removal of the septum) is strongly recommended by both ASRM and ESHRE in women with recurrent pregnancy loss or infertility.
- It significantly improves pregnancy and live birth rates.
2. Bicornuate or Didelphys Uterus
- Surgery is not routinely recommended, as evidence does not show improved outcomes.
- In severe cases (e.g., repeated losses), metroplasty (reconstructive surgery) may be considered—but this is very rare in the modern Western approach.
3. Unicornuate Uterus
- No surgical correction is available.
- Management is focused on monitoring pregnancy closely due to higher risk of complications.
4. Arcuate Uterus
- No specific treatment is necessary.
5. Aplastic/Hypoplastic Uterus
- Uterine transplant or gestational surrogacy may be the only path to biological parenthood.
Hope and Next Steps
If you’ve been diagnosed with a Müllerian anomaly, know that many women with these conditions go on to have successful pregnancies —often with medical guidance or minor surgical correction. The key is an accurate diagnosis, a personalized treatment plan, and a supportive care team.
Ask your fertility specialist if an evaluation for a uterine anomaly is appropriate in your case—especially if you’ve hadmultiple miscarriages, failed IVF cycles, or early pregnancy losses. With the right care, your dream of parenthood is still very much within reach.