Dr. Walid Saleh on Anti-Mullerian Hormone (AMH)
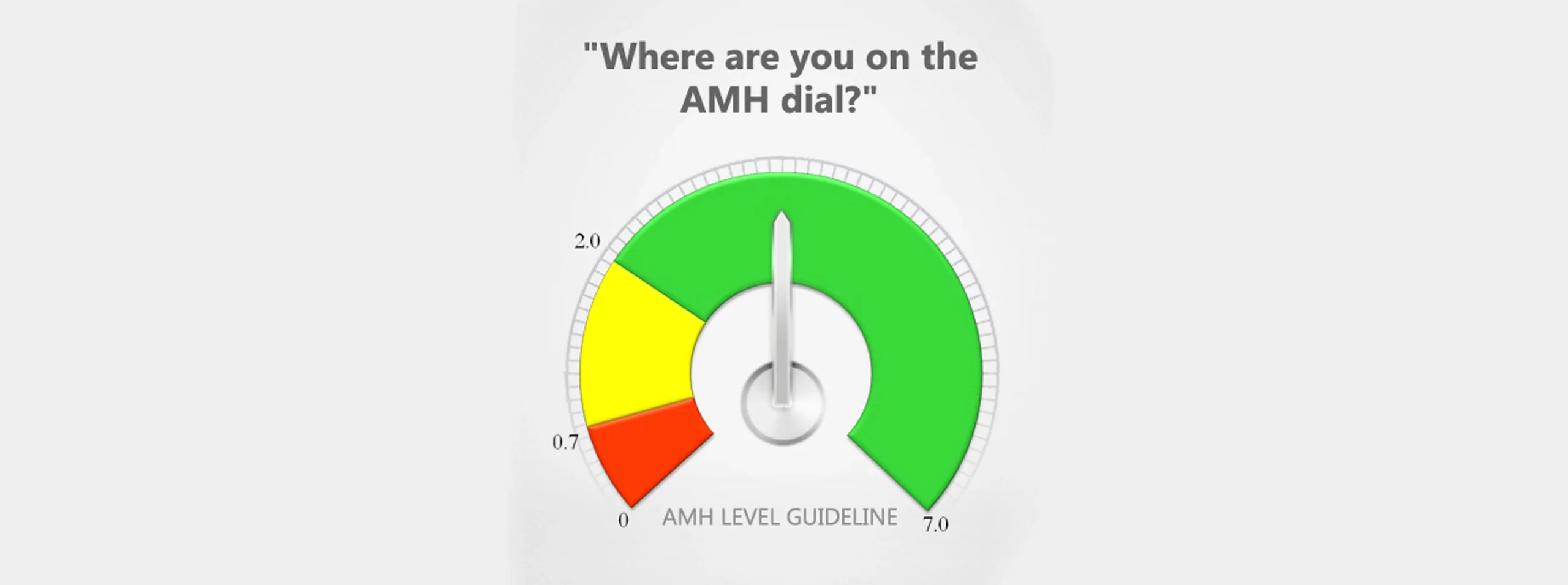
Anti Mullerian Hormone (AMH) is secreted directly by granulosa cells surrounding the oocyte (egg) and is measurable in serum. Because AMH reflects ovarian reserve, it decreases progressively over the reproductive years. Unlike FSH, inhibin-B and estradiol measurements, it is quite stable during the menstrual cycle and can be measured any day of the cycle. Because of its direct ovarian origin, AMH levels may be slightly lower in women taking oral contraceptive.
Women with polycystic ovary syndrome (PCOS) show increased development of antral follicles compared with normal women. Accordingly circulating AMH levels in women with PCOS are two to three times higher than healthy controls.
Recent clinical reports have shown that AMH, a serum marker measuring ovarian reserve, might be better at predicting ovarian response during ovulation induction than current available markers like follicle-stimulating hormone (FSH), inhibin B, or antral follicle count (AFC) by ultrasound. Routine measurement of AMH assists in the individualization of treatment strategies, prediction of poor response and ovarian hyperstimulation syndrome.
It is extensively recognized that IVF pregnancy rates are mostly related to egg quality rather than quantity. While AMH reflects mostly ovarian reserve (quantity), it may also indicate poor egg quality in older women. The relation is not as clear in younger women with decreased ovarian reserve due to surgical removal of one ovary or accelerated loss of oocytes due to anti-ovarian antibodies.
Despite the current obsession with “website statistics”, I strongly believe that AMH measurements, similarly to the other ovarian reserve markers, should NOT be used to exclude couples from IVF. Instead, it should be used to maximize their chances by customizing stimulation protocols and IVF strategies accordingly. For example, using a low dose protocol (mini-IVF) with someone with a lower AMH is counter-productive as it would generate a low number of oocytes to choose from. On the other hand, mini-IVF makes more sense in young women with good egg reserve and quality.